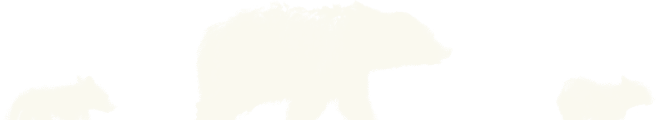
Montana continues to face serious challenges related to drug and alcohol use. Recent state data show rising overdose deaths, with methamphetamine and other stimulants driving nearly half of fatal cases. Alcohol use remains widespread, and the presence of fentanyl in the illicit drug supply has further complicated the crisis. Together, these numbers paint a clear picture: substance-use disorders in Montana are diverse, severe, and increasingly intertwined with mental-health and social challenges.
This growing complexity calls for expanded access to residential programs capable of providing structure, medical supervision, and trauma-informed support. As these statistics illustrate, short-term or limited-scope services often cannot meet the full scale of need.
What the Numbers Tell Us About Treatment Demand
The Rising Impact of Stimulants
While the national conversation often focuses on opioids, Montana’s most persistent issue is methamphetamine. Its link to nearly half of statewide overdoses underscores how stimulant-related treatment must become a central component of addiction care. Treatment programs must be equipped to manage the intense cravings, anxiety, and mood swings associated with stimulant recovery.
Persistent Alcohol and Polysubstance Use
Alcohol continues to account for a large share of substance-use cases across Montana, particularly in rural areas. Many individuals struggle with both alcohol and other drugs simultaneously—a pattern known as polysubstance use. This overlap makes integrated treatment essential, since addressing one substance without the other often leads to relapse.
Treatment Gaps and Access Challenges
Despite high prevalence, treatment access remains limited in parts of Montana. Long distances, workforce shortages, and stigma can delay help for those who need it most. When fewer people receive timely treatment, overdose rates tend to rise. Expanding residential capacity and reducing barriers to care are key steps in closing these gaps.
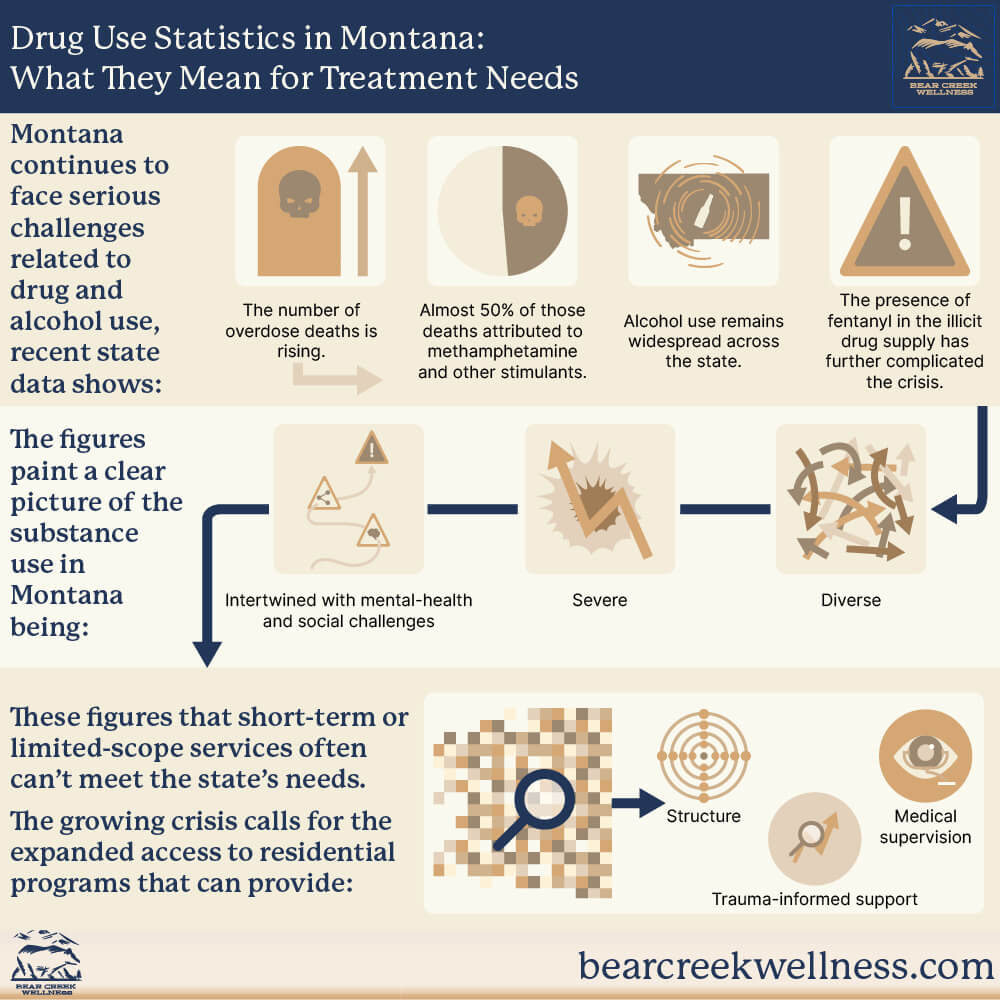
How Data Informs Program Development
Why Residential Programs Matter
Residential programs, such as those offered at Bear Creek Wellness, are designed to meet the level of need reflected in Montana’s data. They provide 24-hour structure, clinical oversight, and peer support in a stable environment—conditions that help individuals focus solely on recovery. This level of intensity is particularly vital for people with severe substance-use histories, trauma, or unstable home environments.
Integrating Mental-Health and Substance-Use Care
Montana’s data also show high rates of co-occurring mental-health conditions like depression and anxiety. Treating these alongside addiction—not after—leads to better outcomes. Integrated residential care allows therapists, medical staff, and clients to address both sets of challenges simultaneously.
Data-Driven Customization
Each trend—whether stimulant dominance, high alcohol use, or co-occurring disorders—guides how programs design their therapies, staff training, and aftercare plans. By aligning services with local realities, treatment centers can ensure residents receive relevant, effective care that meets their specific risks and goals.
What This Means for Treatment Providers Across Montana
Increased Complexity of Client Needs
The average client entering treatment today often presents with multiple layers: mental-health struggles, trauma exposure, housing instability, and chronic relapse patterns. This complexity requires multidisciplinary teams capable of managing both behavioral and medical dimensions of recovery.
Access and Capacity
When overdose rates climb, access to care becomes urgent. Programs must ensure that intake, triage and admission processes are efficient, with minimal delay between identification of need and entry into treatment. Capacity building—especially for residential settings—becomes a key part of meeting the state’s demand.
Bear Creek Wellness: Responding to Montana’s Evolving Needs

At Bear Creek Wellness, every aspect of treatment is built around the realities shown in Montana’s data. As a residential treatment center, Bear Creek offers structure, clinical depth, and holistic healing opportunities that match the intensity many individuals require.
Residents receive care rooted in evidence-based practices like Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT), along with trauma-informed counseling, mindfulness training, and nutrition support. By focusing exclusively on residential treatment—not outpatient—Bear Creek ensures that clients can fully engage in the recovery process without outside distractions or triggers.
The center also leverages Montana’s natural surroundings to promote emotional balance and mindfulness. Nature-based therapy sessions and outdoor reflection help residents reconnect with themselves and their environment—key components of long-term healing.
A Framework for Montana’s Community Response
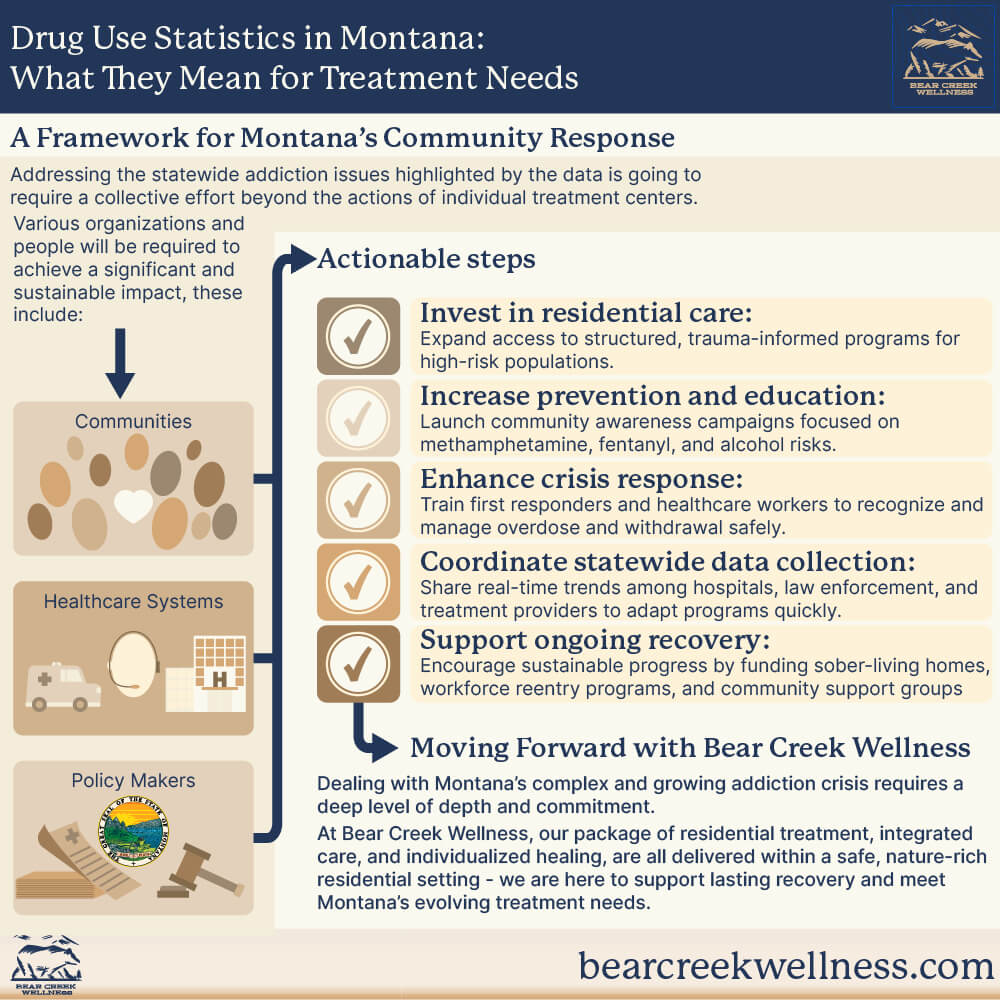
The data emphasize that addressing addiction statewide requires a collective effort beyond individual treatment centers. Communities, healthcare systems, and policymakers can take several actionable steps to reduce overdose risk and strengthen recovery outcomes:
- Invest in residential care: Expand access to structured, trauma-informed programs for high-risk populations.
- Increase prevention and education: Launch community awareness campaigns focused on methamphetamine, fentanyl, and alcohol risks.
- Enhance crisis response: Train first responders and healthcare workers to recognize and manage overdose and withdrawal safely.
- Coordinate statewide data collection: Share real-time trends among hospitals, law enforcement, and treatment providers to adapt programs quickly.
- Support ongoing recovery: Fund sober-living homes, workforce reentry programs, and community support groups to sustain progress after treatment.
Moving Forward with Bear Creek Wellness
The numbers tell a clear story: Montana’s addiction crisis is complex, growing, and deeply tied to mental health and community factors. Programs must respond with the same depth and commitment. Bear Creek Wellness stands apart through its focus on residential treatment, integrated care, and individualized healing—all delivered within a safe, nature-rich setting.
To explore how Bear Creek Wellness supports lasting recovery and meets Montana’s evolving treatment needs, visit bearcreekwellness.com and learn more about our comprehensive residential programs.

Andrea was born and raised in Spokane Washington, she moved to Montana with her husband in 2015. Andrea has been in the field of counseling since 2009. As a licensed addiction counselor, she worked primarily in addiction until 2018 when she completed her master’s degree in marriage and family therapy and became a license clinical professional counselor and a licensed marriage and family therapist. Andrea has worked with diverse populations and found her calling working with individuals and couples struggling with substance use and its relational
impact. With a passion for recovery and healing families, Andrea has built a private practice in Missoula, MT and serves various populations. Andrea’s love for people and her desire to engage with, and promote, internal healing has fostered a truly unique role aiding individualized journeys in recovery. In her spare time, she enjoys her beautiful property west of Missoula with nature at her front and back doors. Her greatest joy in life is spending time with her granddaughter and breaking the cycle of addiction in her own family.